Neuroimaging
Physicians and scientists in the Department of Psychiatry are engaged in a variety of patient-centered neuroimaging studies. Our department currently has a strong focus on neuroimaging projects investigating mechanisms of treatment for psychiatric disorders, predictors of treatment outcomes, and biomarkers of risk. All neuroimaging is performed in collaboration with the Research Imaging Institute (Dr. Peter Fox, Director; RII website: ric.uthscsa.edu), which provides access to fMRI, PET, ERP, and TMS facilities, as well as advanced analysis capabilities. Below, you will find brief descriptions of 5 current neuroimaging projects led by Psychiatry faculty.
Neuroimaging predictors and outcomes of response to stimulant medication
in children with ADHD with aggressive behavior
Dr. Joseph Blader, Ph.D. and Dr. Steven Pliszka, M.D.
A leading reason that children receive behavioral health care is severe emotional dysregulation, seen as a low threshold for behavioral dyscontrol, rage outbursts, and aggression. Most often, youngsters with these difficulties receive a diagnosis of attention-deficit/hyperactivity disorder (ADHD) and are prescribed numerous medications concurrently, including antipsychotic medications. We have conducted clinical trials that show a large proportion of children with severe emotional dysregulation and ADHD experience remission of aggressive behavior with well-monitored, rigorously titrated stimulant medication, which is the first-line pharmacotherapy for ADHD. However, not all children respond to stimulant medication in this way. Possibly, children who do not experience remission of emotional dysregulation with stimulant medications alone may have different underlying neural factors that contribute to their behavioral problems. The goal of our fMRI research is to measure how brain connectivity networks change with stimulant treatment, and to identify neural markers of children who do not respond.
To learn more or to participate, please contact Dr. Blader by email: blader@uthscsa.edu
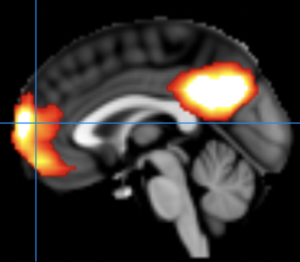
 Changes in Brain Connectivity during Trauma-Focused Therapy for Youth with Posttraumatic stress disorder (PTSD)
Changes in Brain Connectivity during Trauma-Focused Therapy for Youth with Posttraumatic stress disorder (PTSD)
Principal Investigator: Amy Garrett, Ph.D., Associate Professor, Department of Psychiatry & Behavioral Sciences
Trauma-Focused therapy is widely-used and effective for treatment of PTSD in youth, but individualized approaches are needed for the 20% of youth who do not respond sufficiently. Understanding the neural mechanisms underlying psychotherapy for PTSD will help to facilitate the development of individualized therapies. In this study, we are identifying longitudinal changes in brain functional networks that take place during trauma-focused therapy in children and adolescents with PTSD. Participants are randomized to one of two trauma-focused therapies, and functional MRI data are collected several times during the 18-weeks of therapy. Previous data from a similar study by the P.I. have shown that symptom improvement during therapy is associated with normalization of function in the frontal cortex, cingulate cortex, hippocampus, and amygdala. The current study will add to this information by identifying when during therapy these changes take place.
This study is funded by grants from the Baptist Health Foundation and the National Institute of Mental Health.
For more information or to participate in our study, please email the study coordinator at TraumaStudy@uthscsa.edu
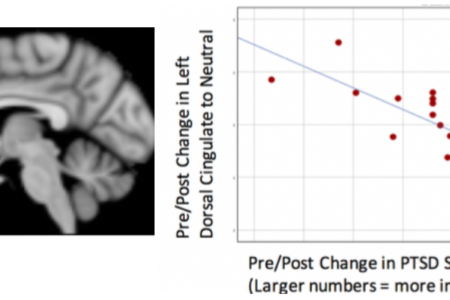
 Functional Neuroanatomy of Social Rejection and Perceived Internal Threat in Anxious Youth at High Risk for Bipolar Disorder
Functional Neuroanatomy of Social Rejection and Perceived Internal Threat in Anxious Youth at High Risk for Bipolar Disorder
Principal Investigator: Donna Roybal M.D.
Longitudinal studies suggest that youth at high familial risk for bipolar disorder experience significant symptoms of anxiety before they develop mood dysregulation. Anxiety is therefore an important symptom in the developmental trajectory of BD, both as a comorbidity and as a potential early predictor. One of the main sources of anxiety in youth is social relationships, which greatly influence an adolescent’s perceived quality of life. However, little is known about the neural underpinnings of social cognition in youth at high-risk for BD, nor how everyday social interactions affect anxiety and emotion regulation, which is a hallmark of BD. In 2 previous studies led by Dr. Roybal (Lilly Pilot Research Award and Hogg Foundation of Mental Health), we showed abnormalities in brain activation and connectivity during a social rejection task in youth with BD. Our current study is using the same social rejection task to evaluate the neural mechanisms of social rejection threat in youth at familial risk for BD who have significant symptoms of anxiety but who have not yet developed symptoms of mood dysregulation. We aim to establish a biological framework with which to predict and prevent the onset of bipolar disorder in children at high familial risk. This study if funded by the NIMH through a K23 grant to Dr. Roybal
For more information or to participate in our studies, see our website:
http://caarebd.com/
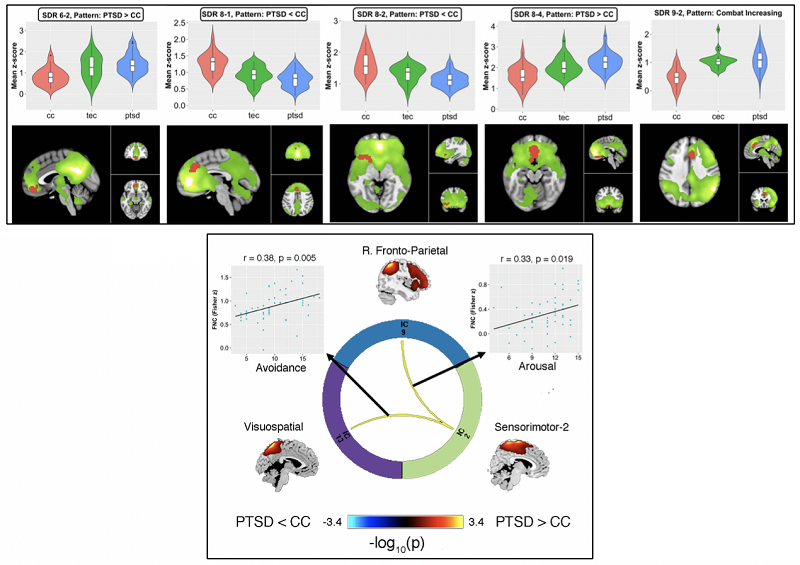
Combat-Related Posttraumatic Stress Disorder: A Group-Wise, Pre-Treatment, Resting-State Network Comparison to Combat-Exposed and Civilian Controls
Resting-state functional magnetic resonance imaging (rs-fMRI) is an emerging means of understanding the neurobiology of posttraumatic stress disorder (PTSD). In a study affiliated with the STRONG STAR consortium performed at the Research Imaging Institute (Peter Fox, PI), a rs-fMRI network analysis was applied to 51 active-duty service-members with PTSD, 29 combat-exposed controls (CEC), and 25 civilian controls without trauma-exposure (CC). Many networks demonstrated intra-network connectivity effects related to combat-exposure and were not specific to PTSD. Yet, PTSD symptoms were significantly correlated with connectivity abnormalities in a subset of regions, mostly confined to cognitive networks, replicating prior reports. Inter-network connectivity of a sensorimotor network and its association with specific symptom clusters was a novel finding. Not only do these results improve the neurobiological understanding of PTSD and combat exposure, but they may serve as clinical biomarkers or even targets for therapeutic intervention.
 Network Dysregulation Among Individuals with Co-Morbid Tinnitus and PTSD
Network Dysregulation Among Individuals with Co-Morbid Tinnitus and PTSD
Psychiatric distress caused by PTSD may increase attention toward tinnitus , as well as perceived loudness and discomfort. It is important that we understand how tinnitus-related distress and PTSD negatively interact together, in order to develop more effective therapeutic approaches. By examining symptoms and brain activity using functional magnetic resonance imaging (fMRI), both before and after receiving therapy for PTSD, we hope to gain the necessary knowledge to develop effective interventions for our nations’ Veterans. This grant is funded through the National Center for Advancing Translational Sciences, National Institutes of Health, through a KL2 grant to Principal Investigator John Moring, Ph.D.
For more information, please contact Dr. Moring at 210-562-6716, or email: MoringJ@uthscsa.edu