Section I: Context of Inpatient Services for Behavioral Health Disorders
Historical Perspective on the Confinement of Individuals with Behavioral Health Disorders
Severe disturbances of emotion, thought, and behavior are prevalent in all human communities, and are among the leading sources of disability, morbidity, and suffering in every age group worldwide. The personal discomfort and dysfunction they cause are compounded by their wider adverse impacts. The latter includes harmful and unsettling behaviors, which can lead to greater social marginalization, disrupted relationships, and other hardships.
The terms for these conditions as a group have shifted over time, to some extent reflecting each era’s understanding and attitudes toward them. Widely-used used terms in recent times include mental disorders or illnesses, psychiatric disorders, brain or neuropsychiatric disorders, and behavioral health disorders. The latter is perceived as less pejorative than the alternatives, and, consistent with the usage of other relevant state and local government documents in Texas, is preferred in this report.
At the most general level, the prevailing scientific view of behavioral health disorders is that (a) vulnerability arises through abnormalities of the brain that are intrinsic (e.g., genetically-based) or acquired through events that damage it; (b) their onset, course, and outcomes are influenced by experiential factors, interventions, one’s other personal characteristics, and the environment; and, (c) some experiences in extremis – such as trauma – can be sufficient to precipitate significant disturbances.
Today’s understanding of these conditions reflects the cumulative research and experience, especially that acquired in the last 130 years or so. The current view of behavioral disorders as treatable, rather than progressively deteriorating or intractable, arose amidst the development of medicinal and other therapies whose beneficial impacts would have astonished earlier generations. Until quite recently, developed societies set those afflicted with severe behavioral health disorders apart from the community, usually to live out their days in grim yet minimally protected circumstances.
Centers that provided compassionate and humane care for the mentally ill flourished intermittently since classical times. For instance, healing temples offered care and serenity, at least for the elite of these societies. Priests, perhaps exploiting a person’s delusions, impersonated gods to provide patients with reassurance or to command changes in behavior. Ancient Greek physicians are thought to have been among the first to offer physiological explanations for behavioral disturbances to replace supernatural ones. However, such proto-scientific views fell in and out of favor in various societies over the centuries that followed.
For most of Western history, however, the treatment of people with psychiatric illness was among the more deplorable of human undertakings. One influential Roman, Aulus Cornelius Celsus (25 BC – 50 AD), advocated a calm environment, encouragement, and herbal remedies for melancholia (4). However, for agitated behavior he called for punitive measures:
‘If however, it is the mind that deceives the madman, he is best treated by certain tortures. When he says or does anything wrong, he is to be coerced by starvation, fetters and flogging… To be thoroughly frightened is beneficial in this illness.” (p. 303)
This strain of thought sanctioned a range of odious practices toward people with severely disordered behavior for centuries to come. In medieval times, demonic explanations for aberrant behavior and thought resurged and motivated the confinement, persecution, shackles, and harsh and neglectful treatment that dominated until the late 18th century. Around that time the leadership of a few institutional facilities for the behaviorally disturbed catalyzed changes whose legacy we inherit as the basis for hospital care of those with severe behavioral disorders.
The contemporary model of the psychiatric hospital originates with reforms during the 1790s. In Britain, William Tuke, founded the York Retreat, which in turn influenced Benjamin Rush in America. In France, Philippe Pinel at the Bicêtre and Salpêtrière Asylums introduced human care rather than physical restraints. In Italy, Vicenzo Chiarugi at Florence’s Hospital of Bonifazio similarly reformed clinical practices. All of these men’s writings contributed to the modern approach to classifying psychiatric illness based on lucid descriptions of symptoms and observed course. In the United States and Britain facilities for the care of those with chronically debilitating mental illness ultimately became a function of local government. Reformers such as Dorothea Dix in the U.S. were instrumental in improving the facilities and standard of living for those destined to spend much of their lives in them.
The larger historical context of psychiatric hospitalization, and enduring apprehensions about the people who need it, continue to imbue inpatient psychiatric care with arguably the most negative stigma among medical treatments today.
This wave of reform and the infusion of public investment, along with an optimistic view that more humane treatment would also cure patients, helped stimulate a significant growth of institutions for the mentally ill beginning in the mid-1800s.
Texas was part of this trend. Austin State Hospital was established in 1854, SASH was established as the “Southwest Insane Asylum” by an act of the Texas Legislature in 1889. We are indebted to the research of Franklin Redmond, M.D. who documented the early history of SASH (5) The current site in southeast San Antonio was chosen based on a number of requirements set by the Legislature, including, “…its accessibility and convenience to the greatest number of inhabitants, the supply of water, building material and fuel, drainage, fertility of the soil [as the hospital would have its own farm], together with railroad connection; and the same shall contain not less than 640 acres…”. The initial building was to have the capacity of 500 patients, at a time when San Antonio had 37,673 residents. Sadly, Section 10 of the Bill rings true to use today:
“Sec 10. The fact that there is a large number of insane persons in the jails of the state who are in need of immediate treatment, creates an emergency, and imperative public necessity exists which requires suspension of the constitutional rule which requires bills to read in each house, and said rule is hereby suspended..”
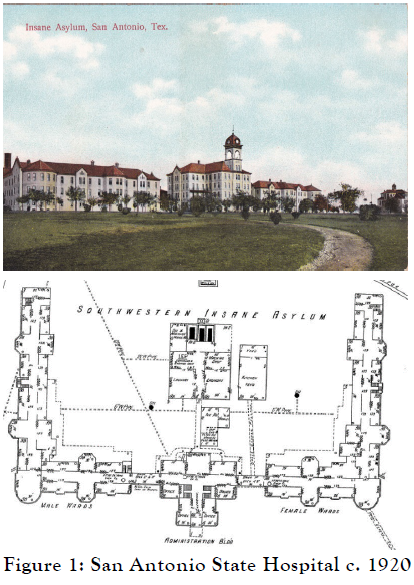 The facility opened on April 6, 1982. The central administrative building was flanked by three story wards on each side, segregated by gender.
The facility opened on April 6, 1982. The central administrative building was flanked by three story wards on each side, segregated by gender.
A novelty for its day, the facility had open wards rather individual cells. This favorably impressed a reporter from the San Antonio Daily Express (forerunner of the Express-News) who wrote on August 26, 1894:
“Instead of finding them confined to narrow cells, they are allowed to roam at will throughout broad corridors and halls with regular outings twice day…the inmates were seen sitting about the corridor or congregated in the large open apartments in the center of the room where they talked together, played or did what they saw fit.”
Dr. W.L. Barker, the superintendent, remarked how the layout of the hospital reduced the violence of patients and the need for “severe” treatment, stating proudly that a straitjacket had not been applied in six months (5, p. 34). Five new buildings were completed by 1939, several of which are still in use today. One unit, built in 1934, serves as the Adolescent Unit.
It was almost inevitable, though, that the burdens of increasing urbanization and migration, economic dislocation, and the infectious epidemics of subsequent eras, along with the fact that more humane care was not necessarily curative, combined to strain these resources. Underfunding, public discouragement and a growing patient population degraded many publicly supported facilities into quite dismal places well into the 20th century. By 1955, over 550,000 individuals lived in inpatient psychiatric facilities in the United States, or about 300 per 100,000 Americans. In 1940, the patient population at SASH was 2,854 with a waiting list of 700 in the state jails (5). By 1950, although definitive census figures are difficult to find, Redmond (5) estimates that number grew to between 3,500 and 4,000 with no additional building during that period. This nationwide overcrowding and neglect facilities enabled the image of the psychiatric hospital in popular culture as a “snake pit” to take root, and depictions like those shown in One Flew Over the Cuckoo’s Nest to epitomize them. One tragedy of this era is that these images largely upended earlier progress that transformed psychiatric hospitals to becoming widely perceived as humane places for healing, not of imprisonment and abuse.
Beginning in the early 1960s, however, several trends contributed to the depopulation of state hospitals throughout the United States. The development and widespread use of effective pharmacotherapeutic agents for psychosis and major mood disorders finally turned the tide, and the age of “asylum psychiatry” began its descent. The creation of Supplemental Security Income (SSI) and Medicaid meant that persons with severe mental illness could afford to live and seek medical care in the community. Elderly patients with dementia could have nursing home care funded by Medicaid. In 2014, all psychiatric beds combined (acute and long-term, private and public) would account for 33 per 100,000 people.
During the same period, vigorous advocacy, progress in treatment, and the deinstitutionalization movement culminated in the Community Mental Health Act (CMHA) of 1963. The growth of local, smaller inpatient psychiatric units caused hospitalizations to be regarded as a time-limited health service, rather than a custodial setting far from home for disorders that caused lifetime disability. Acute-care units in general hospitals proliferated, where comparatively short stays for episodic crises became the norm. Nevertheless, the ambitious aims of the CMHA were never fully funded, and it is unlikely that adequate outpatient supports ever existed to offset the reduction of inpatient beds for those with severe behavioral health disorders. Despite treatment advances and a transformation in both lay and scientific understanding of behavioral health disorders, the historical context of psychiatric hospitalization, and enduring apprehensions about the people who need it, continue to imbue inpatient psychiatry with arguably the most negative stigma among medical treatments today.

Rate per 100,000 adults.
Inpatient treatment remains vital to a system of care that calibrates interventions with one’s current needs. Although contemporary treatments and other supports alleviate many of their hardships, behavioral health disorders remain chiefly chronic conditions whose severity and impairment often fluctuate. Exacerbations that threaten safety or signal alarming changes in mental status often require inpatient care. Advances in pharmacotherapies, psychosocial treatments and rehabilitative methods combined with a broad commitment – ideologically if not always fiscally – to community-based care had nourished a hope that restrictive treatment settings like hospital wards would become anachronisms. Ongoing outpatient treatment that is timely, consistent, effective and utilized as prescribed may reduce the crises that result in inpatient care, but, on a population level, current interventions do not eliminate them. Regrettably, those with psychiatric disorders are still overrepresented in the nation’s jails and prisons; trends shown in Figure 2 leads to a plausible inference that the depletion of inpatient behavioral health capacity contributed to the steep rise in the incarcerated population. 130 years after the Texas Legislature established SASH, the need to provide timely care in secure settings persists.
Recent developments in the United States have provoked widespread concerns that there is a shortage of hospital-based inpatient care resources for behavioral health disorders. Along with other trends, these developments have impacted, if not transformed, the role of state hospitals. We now turn to describe these developments because they are relevant to our consideration of how a reinvigorated San Antonio State Hospital can best serve the residents of South Texas.
Recent Developments and the Role of State Behavioral Health Facilities in Today’s Continuum of Care
1. Ultra-Short Stays and Serial Admissions in Acute-Care Hospital Settings
In the 1980s and early 1990s there was immense growth in private psychiatric hospitals, resulting in a period of oversupply and overutilization. From the mid- 1990s, however, vigorous cost-containment and utilization authorization requirements for care led to a significant paring of the nation’s behavioral health inpatient care capacity. Payers implemented more stringent criteria to approve admissions for which they would reimburse costs, and ongoing review had the effects of dramatically reducing lengths of stay. Average lengths of stay became markedly shorter, reflecting the view that acute-care inpatient treatment serves a crisis stabilization role, with patients transitioning to outpatient care as soon as extreme behavioral disorganization, emotional volatility, agitation, or suicide risk seems to abate. This approach eclipsed the goal of ensuring that treatments implemented in the hospital were likely to yield remission or at least a durable reduction in symptoms.
At the same time, the number of admissions to acute-care settings rose, most significantly for children and adolescents. In principle, more admissions and shorter lengths of stay could be a good thing – there may have been a high demand for inpatient care that was unfulfilled because of needlessly long lengths of stay reducing availability. Instead, however, it appears that for many seriously ill patients the result is a “revolving door”. Among patients with psychotic disorder, the current care paradigm might be justifiable for early phase treatment, where lower doses of antipsychotic agents are helpful and the likelihood of good response emerging within two weeks is higher. But with more episodes, chronicity, and suboptimal response to medications, short stays become counterproductive. After 14 days of unsatisfactory response to antipsychotic therapy, the probability of a robust response with continuation drops significantly. In these situations, short stays typically result in layering of additional medications, since there is little time nor inclination to risk discontinuation of a treatment that may not be beneficial.
Locally, there are some indications that short hospital stays are also associated with sooner and more frequent likelihood of rehospitalizations. Comparing short-term patients, readmission rates are lower for patients discharged from a state hospital than from a contracted bed, reflecting greater challenges in maintaining close communication and coordination with private psychiatric hospitals.
2. Recovery, Not Just Symptom Reduction, is the Goal of Behavioral Health
As public-sector behavioral health strives to meet the challenges in caring for people who have severe illnesses, today’s aspirations for treatment outcomes embody a quality of life that is satisfying and meaningful, ideally approximating as near as possible what one would experience if unencumbered by illness. This principle is the core of today’s emphasis on recovery (6). HHS’s Behavior Health Services’ vision statement now incorporates that goal: “Hope, resilience and recovery for everyone”.
The concept of recovery in mental health was initially developed by service users and has led to disparate conceptualizations but broadly refers to ‘a way of living a satisfying, hopeful, and contributing life even with limitations caused by illness’, while developing new purpose or meaning. The importance of addressing service users’ personal recovery alongside more conventional ideas of clinical recovery is now supported in guidance for all key professions (7).
In practical terms, organizations with a recovery orientation strive to promote autonomy and individuality, informed choice, peer support, focus on strengths, integration in community life and workforce, and service quality improvements. The axiom that behavioral health services should be available “at the right time, in the right place, and with the right resources” has long been endorsed in principle by nearly every service organization and government. The recovery movement’s significance partly stems from its emphasis that the “right” things promote individual recovery, not just temporizing measures that suppress symptoms but leave individuals adrift because they lack the supports to lead a productive and meaningful life.
The experience, threat, or witnessing of extreme harm, especially interpersonal violence, is a risk factor for behavioral health disorders. Growing appreciation of this relationship has led to a related principle, that recovery for many individuals must include interventions that take account of traumatic experience, as well as resources to alleviate post-traumatic stress disorders per se. Many aspects of such trauma- informed care include processes that most would agree should be part of treatment for everyone. For instance, the Substance Abuse and Mental Health Service Administration’s (SAMHSA) guidance on trauma-informed care includes six principles: safety, trust and transparency, peer support, collaboration and mutuality, promoting autonomy (empowerment, voice, and choice), and appreciation of an individual’s context (cultural, historical and gender issues). But trauma-informed care also means the development of therapeutic environments that factor in how certain features.
3. Reduced Capacity for Inpatient Behavioral Health Care
The successes of psychiatric therapies to relieve debilitating symptoms and enable those affected to lead more independent lives are remarkable scientific and public health achievements. However, there is widespread concern that the move away from hospital-based services may have gone too far. In the U.S., a growing consensus is that the shortage of inpatient resources that resulted has adverse impacts (8). Reduced capacity of publicly-supported facilities seems to have been especially severe. For example, between 1970 and 2014 state and county psychiatric hospital beds decreased 93% (9). In Texas between 1982 and 2010, such beds declined by 36%. Some observers have implicated the general trend toward fewer inpatient beds to rises in incarceration of those with behavioral health disorders and rising suicide rates (10,11), though a direct causal connection is controversial.
Naturally, a major driver of these trends is cost. In fiscal year 2015, states spent $9.4 billion to operate psychiatric facilities, representing 23% of total state mental health agency expenditures. Averaged over total state hospital bed capacity nationwide, that equates to more than $242,000 annually per patient. Medicaid’s Institution for Mental Diseases exclusion (IMD) prohibits cost recovery for patients aged 22-64 in larger (> 16 beds) inpatient behavioral health facilities, although some states have obtained waivers. Federal Mental Health Block Grants cannot be used for inpatient services. These factors contributed to states encouraging the development of inpatient services in general hospitals, where Medicaid would reimburse treatment. However, declining reimbursement from payers to private hospitals for this service makes conversion of beds to other purposes financially attractive.
“Rightsizing” inpatient capacity in various types of behavioral health contexts (acute, longer-term, crisis stabilization, forensic services) is difficult. Need is partly a function of alternative care availability and other safety-net services. Compounding these challenges, population dispersion in a large state makes it hard to efficiently have state hospital services at distances advantageous to patients and families.
4. State Hospitals Fill the Gap for those Needing Longer Episodes of Inpatient Care
Until about 15 years ago, state behavioral health hospitals’ role in the continuum of care was to provide a safe and therapeutic environment for individuals with disorders for which improvement was likely to be gradual at best. However, the shift toward reduced inpatient behavioral health capacity and shrinking lengths of stay in nearly all facilities has led to state hospitals filling the need to care for those having less chronic illnesses but who need hospital level care to establish an effective treatment regimen. Often, either the intrinsic severity of their disorder or a lack of supports causes them to need 24-hour care until treatments gain traction. This may mean discontinuing treatments, titrating others, and establishing core skills to resume care in outpatient settings, neither of which one-week hospitalizations are suited for. The timeframe to initiate and safely optimize pharmacotherapy for patients who already had insufficient response to treatment is, realistically, at least one to two months. State hospital services have increasingly become the site for individuals requiring this length of stay to attain remission adequate to resume outpatient care and community living.
Locally, San Antonio State Hospital has assumed this role. Many stakeholders agreed that SASH is excellent at providing extended stabilization services for people with complex and difficult-to-treat disorders, usually psychotic illnesses, frequently with concurrent substance abuse. These extended stabilization services were identified as a critical component of the care system that needs to continue into the foreseeable future. Family members of former patients also pointed out the need for continuing extended stabilization services, stating that acute care provided in private hospitals often does not provide the stability their loved ones need; they often cycle through emergency rooms and inpatient stays because of a lack of extended care that could be provided by SASH. As one stakeholder stated, “All beds are not created equal.”
5. State Hospitals Provide Care and Shelter for the Very Ill who Lack Safe Alternatives even after Lengthy Hospitalization
Even with optimal care and adherence, current treatments are insufficient for a number of individuals with severe, treatment-refractory conditions. Many of these patients would not be safe residing in even supervised group home settings, or lack skills that would be expected of them in these or other supported living arrangements. At the present time, the state hospital continues to be, in effect, their home.
Many inpatients then become elderly. As they become progressively more disabled, both physically and by virtue of pernicious psychiatric illness, the range of care alternatives is frequently unsuitable. Compounding these problems is the dwindling availability of kin who might have played at least some role in helping with transfer to a less restrictive setting.
The severity of the patients at SASH is illustrated by the following case study (identifying data removed):
YR, a 45-year-old man with schizoaffective disorder, was admitted to SASH on a forensic commitment. He is charged with attempted sexual assault of hospital staff; he exposed himself and asked to have sex with a female. He had eloped from a small group of patients that were being escorted from one unit to another in the same building.
YR has a long history of sexually provocative and aggressive behavior plus treatment-refractory delusions that include his affiliation with popular music groups. He was first admitted to a state hospital nearly 25 years ago and has been in various facilities almost continuously since. Even before then, he had numerous psychiatric hospital admissions in other states dating from adolescence. YR has a supportive family. His brother is an accomplished professional and serves as his legal guardian. One sister is a nurse. They relate that YR was quite intelligent and outgoing prior to a traumatic event as a preteen—he was raped by a gang.
His illness has proved very difficult to treat. An extensive array of medication trials has yielded only minimal benefits. He currently resides on the hospital’s psychiatric intensive care unit, which is designed for the most aggressive and disturbed patients. He has made no progress in terms of attaining competency regarding his criminal charge and is unlikely to ever do so.
YR requires physical restraint by staff on almost a daily basis, often 2-3 times per day. He is profoundly intrusive and insists that essentially all food items and the personal possessions of other patients belong to him. He remains sexually disinhibited. Still, at times he is articulate and able to joke with staff.
6. State Hospitals are Increasingly Used by Government for Criminal Justice Mandates
The increase in the past 10 years or so in the use of state hospital beds for defendants undergoing evaluation or treatment because a criminal court must address whether they are competent for proceedings to continue is major development nationwide. In many localities, it is perceived as an encroachment on the public health system that is thwarting limited inpatient capacity to fulfill its clinical mandate (9,12) The impact on SASH’s clinical mission is significant and compels discussion in several sections of this report.
Briefly, adjudicative competence or competence to proceed is a legal construct that refers to an accused person capacity to participate in proceedings related to an alleged criminal offense (13,14). Competency to stand trial is used practically as a synonym, although the competence at issue pleas without trials, ability to share with counsel exculpatory information, ability to exercise one’s right to withhold self-incriminating material, and ability to participate in other legal processes (14). The requirement that defendant possess understanding and capacity to defend himself or herself against accusations has long been part of Anglo-American legal doctrine. The specific elements in the determination of competence in this country come from a Supreme Court decision, Dusky v. U.S., in 1960. The Court determined that the tests for competence to stand trial are whether the defendant has “sufficient present ability to consult with his lawyer with a reasonable degree of rational understanding—and whether he has a rational as well as factual understanding of the proceedings against him”. Competence is also a characteristic of the person to participate in proceedings now, unlike determinations of not guilty by reason of insanity, which is a determination of the person’s state of mind at the time of the offense.
States differ in some important aspects of how competence is ascertained and what follows a determination of incompetence. In general, if charges are not dropped, defendants can be remanded for treatment to “restore competence” (notwithstanding that the term is a misnomer for individuals have never fully possessed such competence in their adult lives). Several decades ago, when commitments for individuals found incompetent to stand trial (IST) were used more sparingly, such treatment occurred almost exclusively on inpatient psychiatric settings. More recently, competency restoration may take place, at judicial discretion, on an outpatient basis (OCR), within a detention facility (jail-based competency restoration; JBCR), or in an inpatient setting. Some states limit the range of alleged offenses for which inpatient commitment may be ordered, given that such placement does deprive one of liberty for charges that could, in other circumstances, result in posting bail or other pretrial release terms.
Growth in non-dismissed charges against those found IST contributed to a swelling of the incarcerated and psychiatrically hospitalized population by nonsentenced individuals. Suits brought against state agencies in Federal courts successfully argued that those found IST have a right to be treated in a hospital rather than correctional setting (e.g., Trueblood et al. v. Washington State DSHS). This further increased demand on public hospital services. Although there has yet to be a ruling with nationwide applicability, the trend in Federal district and appellate courts has led many state mental health planning authorities to take notice of the settlements reached in these cases, and to take proactive measures that insure timely access to appropriate care that does not unduly deprive individuals of liberty.
Regardless of where it occurs, competency restoration comprises (1) psychiatric care appropriate for the individual’s illness and (2) education on criminal court procedures. Patients are periodically reassessed to gauge improvements in adjudicative competence, and courts are advised accordingly. A variety of structured evaluation tools are available for these assessments (e.g., the Georgia Competency Evaluation Assessment, the MacArthur Competence Assessment Tool – Criminal Adjudication) though their use is not required by courts in Texas.
7. Summary
The U.S. has shed inpatient bed capacity drastically. In this context of diminishing resources, behavioral health inpatient services operated by state agencies have come under several increasing pressures from:
- reimbursement practices that led other hospital facilities to abandon treatment that is more than minimally necessary to ‘stabilize’ an acutely impaired person;
- rising, yet appropriate, expectations for the role of services in promoting more complete recovery from behavioral disorder than symptom suppression alone; and
- heightened utilization of these facilities by criminal justice systems to admit individuals for adjudicative competence at the expense of other patients whose clinical needs better match the care state hospitals
Accordingly, the state hospital has assumed responsibility for patients who have had serial hospitalizations with brief lengths of stay with little lasting effect on their course of illness. They have also assumed responsibility for patients who have no alternatives to hospital care for safety and functional support, patients who need intensive rehabilitation efforts to prepare for resumption of community life, and ill individuals whose behavior leads to legal entanglements but whose cognitive impairments preclude ordinary criminal justice processes from going forward.
These general nationwide trends combine with the specific inadequacies of San Antonio State Hospital to make its reconstruction and reinvigoration of the greater care system of which it is part one of the most urgent public health objectives in our region today.